Neurodivergence and Substance Use Disorder: Understanding the Intersection

Neurodivergence and substance use disorder are complex topics that intersect in many ways. Many individuals with neurodivergent conditions, such as ADHD or autism, are at a higher risk for developing substance use disorders. The reasons are varied, including self-medication for unrecognized symptoms or difficulties in social environments.
Understanding the relationship between neurodivergence and addiction is crucial for effective prevention and care. Research shows that neurodivergent brains may process substances differently, leading to unique challenges in treatment. For instance, people with ADHD might use stimulants like cocaine to manage their symptoms, only to become dependent on these substances.
Public health strategies need to address these complexities to provide better support and interventions. By recognizing the specific needs of neurodivergent individuals, healthcare providers can develop more tailored and effective prevention and treatment plans. Learn more about how neurodiversity impacts addiction treatment to see the full picture.
Understanding Neurodivergence
Neurodivergence refers to the different ways the brain can function, often leading to varied cognitive processes and behaviors. Key areas include the specific conditions associated with neurodivergence and how both genetic and environmental factors play a role.
Defining Neurodivergence
Neurodivergence encompasses a range of neurological and developmental conditions. Key examples include Autism Spectrum Disorder (ASD) and Attention-Deficit/Hyperactivity Disorder (ADHD). These conditions affect how individuals perceive the world and interact with their surroundings.
- Autism Spectrum Disorder: Individuals with ASD may have difficulties with social interactions and communication. They might also engage in repetitive behaviors and have a strong focus on specific interests.
- ADHD: This involves symptoms such as inattentiveness, hyperactivity, and impulsiveness. People with ADHD may struggle with staying focused, organizing tasks, and regulating their emotions.
Both ASD and ADHD illustrate the diversity in brain function and how it influences daily life and interactions.
Neurodivergent Conditions and Substance Use
Studies suggest a correlation between neurodivergence and increased substance use. For instance, individuals with autism and above-average intelligence are more likely to develop substance dependency. This can be linked to challenges in social interactions and coping mechanisms.
- ADHD and Substance Use: People with ADHD are at higher risk of substance misuse, possibly due to impulsivity and a tendency to seek novel experiences. They may use substances as a way to self-medicate for their symptoms.
- Dual Diagnosis: Having both ASD and ADHD can elevate the risk even further. Managing both conditions is crucial to reduce the likelihood of developing dependency.
Understanding these links can help tailor interventions and support for those at risk.
The Role of Genetics and Environment
Both genetics and environmental factors influence neurodivergence and substance use. A family history of neurodivergent conditions or substance use disorders increases risk due to inherited traits.
- Genetics: Studies indicate a strong genetic component in conditions like ADHD and ASD. Specific genes have been associated with the likelihood of developing these disorders.
- Environmental Factors: External influences such as prenatal exposure to toxins, or stressful family environments, can also impact the development of neurodivergent conditions.
Combined, these factors shape the brain’s structure and function, contributing to neurodivergence. Understanding these influences is key to developing effective prevention and treatment strategies.
Substance Use Disorder Explained
Substance Use Disorder involves the ongoing use of drugs or alcohol despite significant problems related to their use. It affects brain function and behavior, resulting in an inability to control the use of these substances.
Criteria for Substance Use Disorders
The DSM-5 outlines criteria to diagnose Substance Use Disorder (SUD). These include a pattern of use leading to significant impairment or distress with at least two of the following within a 12-month period:
- Using larger amounts or over a longer time than intended.
- Persistent desire or unsuccessful efforts to cut down or control use.
- Spending a lot of time getting, using, or recovering from substance use.
Other criteria involve cravings, problems fulfilling major obligations at work, school, or home, continued use despite social or interpersonal problems, and giving up important activities. A pattern of dangerous use (using substances in risky situations) and physical or psychological problems due to use are also included.
The Spectrum of Substance Use
Substance Use Disorder exists on a spectrum. This spectrum ranges from mild to severe, depending on the number of criteria met.
- Mild SUD: 2-3 criteria met.
- Moderate SUD: 4-5 criteria met.
- Severe SUD: 6 or more criteria met.
Substance Dependence often signifies a more severe form of addiction, involving tolerance (needing more to get the same effect) and withdrawal symptoms. Substance Misuse includes hazardous use without meeting full criteria for SUD but can still lead to negative consequences. Understanding this spectrum is crucial as it shows that not all cases are the same and can vary significantly in terms of severity and impact.
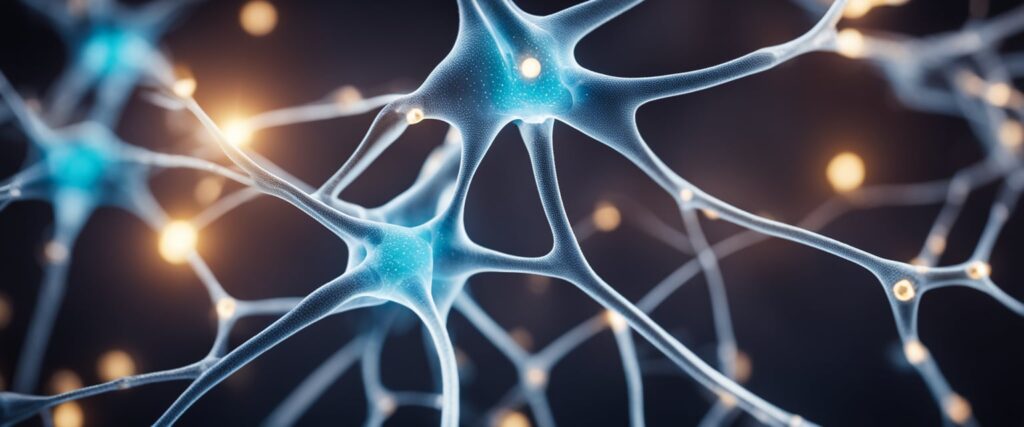
Neurobiology of Addiction
Addiction impacts brain structure, function, and neurotransmitter activity. Key areas include the prefrontal cortex, amygdala, and cingulate cortex.
Neurocircuitry of Reward and Reinforcement
The brain’s reward system plays a critical role in substance addiction. The nucleus accumbens, part of the basal ganglia, is crucial for reinforcing substance use. It interacts with the prefrontal cortex (PFC) and amygdala to create a powerful feedback loop. This loop links rewarding experiences with the urge to seek drugs.
Substances boost dopamine levels in the reward circuit, creating feelings of pleasure. The cingulate cortex also participates by processing emotions related to drug use. This complex neurocircuitry explains why breaking the cycle of addiction is so challenging.
Brain Structure and Function in SUD
Substance use disorder (SUD) affects several key brain regions. The prefrontal cortex (PFC), responsible for decision-making and impulse control, often shows reduced activity in individuals with SUD. This impairment makes it harder to resist cravings and leads to poor judgment.
The amygdala, which processes emotions, becomes overactive, heightening stress and anxiety that drive substance use. The cingulate cortex, involved in emotion regulation, can also show changes in function. These structural alterations underscore the chronic nature of addiction as a brain disease.
Neurotransmitter Activity and Changes
Neurotransmitters are critical in the development of addiction. Dopamine, which regulates pleasure and reward, is significantly impacted. Substances increase dopamine release, reinforcing drug-seeking behavior. Over time, the brain produces less dopamine naturally, requiring more of the substance to achieve the same effect.
Other neurotransmitters like serotonin and glutamate are also affected. Serotonin influences mood and social behavior, while glutamate is involved in learning and memory. Imbalances in these neurotransmitters contribute to the compulsive behaviors seen in addiction, making it a complex disorder to treat.

Comorbidity of Neurodivergence and SUD
Neurodivergent individuals frequently experience comorbid substance use disorders (SUD), which can complicate their mental health. This section will explore the prevalence and mutual influence of these conditions, as well as the assessment and diagnostic challenges they present.
Prevalence and Mutual Influence
Neurodivergence, which includes conditions like ADHD, autism spectrum disorder, and others, often co-occurs with SUD. For example, people with ADHD have a high comorbidity rate with substance use disorders. Research shows that ADHD and SUD share underlying neurobiological factors.
Furthermore, the stress and stigmatization faced by neurodivergent individuals can increase the likelihood of substance use as a coping mechanism. These factors mutually influence each other, making it challenging to treat both conditions separately. SUD can exacerbate symptoms of neurodivergence, while untreated neurodivergence can lead to increased substance use.
Assessment and Diagnostic Challenges
Diagnosing comorbid neurodivergence and SUD is complex. Traditional assessment tools often fail to differentiate between symptoms of neurodivergence and those induced by substance use. This overlap can lead to misdiagnosis or delayed diagnosis.
For example, ADHD symptoms like impulsivity can be mistaken for substance-related behavior. Similarly, cognitive impairments from substance use can mimic traits of neurodivergent conditions. Accurate assessment requires integrating multiple diagnostic approaches and considering the individual’s full psychological history, including both neurodivergent traits and substance use patterns.
Proper diagnosis is crucial for effective treatment, as addressing only one condition can leave the other untreated, reducing overall treatment efficacy. Therefore, a comprehensive and integrated approach is essential for successful outcomes.
Neurodivergent Tests
A neurodivergent test help identify the differences in brain structure and function, often through advanced imaging techniques and behavioral assessments. These tests are essential for understanding how an individual’s brain works and offer insights into potential substance use disorder risks.
Neuroimaging and Diagnosis
Neuroimaging techniques such as MRI (Magnetic Resonance Imaging) and fMRI (Functional MRI) are useful in identifying structural and functional differences in the brains of neurodivergent individuals. PET (Positron Emission Tomography) and SPECT (Single Photon Emission Computed Tomography) scans help highlight areas of the brain that may function differently.
These tools are particularly helpful in spotting abnormalities related to ADHD, autism spectrum disorders, and other conditions. Scientists use these images to understand the brain’s activity patterns, which can offer clues about susceptibility to substance use disorders.
There are online neurodivergent tests, but be mindful that a free online assessment isn’t a replacement for medical advice.
Behavioral and Psychological Assessments
Behavioral and psychological assessments are another essential part of neurodivergent testing. These tests often include self-administered questionnaires and professional evaluations to identify traits of neurodivergent conditions. For instance, the Neurodivergent Test helps people learn whether they have traits of ADHD or autism.
By observing how an individual responds in different scenarios, clinicians can better understand their cognitive and emotional processes. Such assessments are vital for building tailored intervention plans to manage both neurodivergence and potential substance use disorder, ensuring that each individual’s unique needs are met.
Treatment and Management Strategies
Effective treatment and management of neurodivergence in substance use disorder requires a combination of pharmacological interventions, behavioral therapies, and supportive care. Each approach addresses different aspects of the disorder and aids in promoting lasting recovery.
Pharmacological Interventions
Pharmacological interventions can be vital in managing substance use disorder, particularly for individuals with neurodivergence. Medications such as methadone and buprenorphine are often used to reduce cravings and withdrawal symptoms. These medications help to stabilize brain function.
Antidepressants like SSRIs are sometimes prescribed to manage co-occurring mental health conditions. Novel treatments such as those targeting specific neurotransmitter systems are also showing promise in treating addiction by enhancing resilience and motivation.
Close medical supervision is necessary to avoid potential side effects and interactions. Individuals should follow a treatment plan tailored to their unique needs for the best outcomes.
Behavioral Therapies
Behavioral therapies are essential in treating substance use disorder, especially for those with neurodivergence. Techniques such as Cognitive Behavioral Therapy (CBT) help individuals recognize and modify harmful patterns of thinking and behavior. Dialectical Behavior Therapy (DBT) is useful for managing intense emotions.
Motivational Interviewing (MI) aims to boost a person’s intrinsic motivation to change, which is crucial for long-term recovery. Group therapy provides a space for shared experiences and support.
Incorporating neurodivergent life hacks can also be beneficial. For example, keeping a recovery journal can help track progress and recognize triggers. Apps that provide reminders and coping strategies can be a part of day-to-day management.
Supportive Care and Rehabilitation
Supportive care is an important aspect of managing substance use disorder in neurodivergent individuals. This includes access to comprehensive rehabilitation programs that provide stability and support during recovery. These programs often offer a combination of medical, psychological, and social services.
Creating a strong support network is crucial. Family therapy can help repair relationships that have been strained by addiction. Support groups like 12-step programs provide a community of individuals with shared experiences.
In daily life, establishing routines and using organizational tools can make a big difference. Simple tools like planners or digital calendars can help manage time and reduce stress, promoting a healthier lifestyle.
Relevant resources like the CDC’s guidance on treatment of substance use disorders and strategies from the American Medical Association offer further insight into comprehensive care options.
Challenges and Considerations
When dealing with neurodivergence and substance use disorder, several key challenges arise, including maintaining compliance and preventing relapse, addressing social and legal implications, and guiding future directions in research and treatment.
Compliance and Relapse Prevention
Maintaining compliance with treatment is crucial for individuals with substance use disorders and neurodivergence. Stress can significantly impact their ability to adhere to treatment plans. It’s essential to have personalized strategies, as traditional methods may not work well for them. Routine monitoring and flexible treatment plans can help.
Relapse prevention also requires tailored approaches. The neuropathways involved in addiction may be different in neurodivergent individuals. Identifying triggers and providing ongoing support are vital. Behavioral therapies and involving family members can improve outcomes.
Key strategies:
- Personalized treatment plans
- Regular monitoring
- Family involvement
Social and Legal Implications
Social stigma is a major barrier for neurodivergent individuals with substance use disorders. They often face discrimination, making it harder to seek help. Raising awareness about neurodiversity can reduce stigma and encourage more people to seek treatment.
Legal issues are another concern. People with these disorders may encounter the criminal justice system. They often need legal advocacy and support. Ensuring they receive appropriate treatment instead of punishment is crucial.
Important considerations:
- Reducing stigma
- Legal advocacy
- Access to appropriate treatment
Future Directions in Research and Treatment
Future research should focus on understanding the unique neurobiological aspects of neurodivergent individuals with substance use disorders. Using advanced neuroimaging techniques can reveal the specific brain changes involved.
Treatment methods need to evolve based on research findings. Developing new therapies that target the unique needs of neurodivergent individuals is essential. Collaborative efforts between neuroscientists, clinicians, and policymakers can drive these advancements.
Research priorities:
- Advanced neuroimaging
- Developing targeted therapies
- Collaboration among experts
Support Systems and Resources
Effective support systems and resources are essential for addressing neurodivergence and substance use disorder. These can include family and community support, online aids, and healthcare professional networks.
Family and Community Support
Family and community support are key in helping individuals with neurodivergence and substance use disorder. Families provide emotional backing, stability, and practical assistance. For instance, family members can help manage daily routines and offer moral support through recovery processes.
Community support groups offer a sense of belonging and understanding. These groups provide a platform where individuals can share experiences and receive guidance. They often run programs that foster a supportive environment, helping individuals stay engaged and motivated.
Peer support from others who have faced similar challenges is also beneficial. They can offer advice, share coping strategies, and serve as role models for recovery.
Online and Technological Aids
Online and technological aids are crucial resources for people dealing with these issues. Numerous apps and websites offer educational content, self-help tools, and peer support forums.
For instance, forums on websites like The Raleigh House provide platforms where individuals can connect and support each other. Apps focused on mental health and substance use recovery offer tracking tools, mindfulness exercises, and direct links to professional help.
Virtual therapy sessions offer flexibility and can be less intimidating than face-to-face meetings. They provide an essential resource for those who may have mobility issues or feel uncomfortable in traditional settings.
Healthcare Professional Networks
Individual therapy sessions, group counseling, and medical treatments are integral parts of these networks. Neurobiology research has shown the importance of treating both neurodivergence and substance use simultaneously for better outcomes.
Healthcare professionals can also connect individuals with local resources, including detox programs and rehab facilities. These structured programs are designed to provide comprehensive support and continuous care throughout the recovery journey.
Healthcare professional networks offer specialized and structured support. These networks consist of doctors, therapists, and other healthcare providers trained to address both neurodivergent conditions and substance use disorders.